We started the day out heading to a clinic approximately 2 hours away from the hotel. It was a bumping ride (musically and physically). We first went to a very small clinic about an hour from the main road, Rokulan community health center. The clinic was run by  Francis, a community health officer (CHO) and the community supervisor for the four peripheral health units (PHUs) in the neighboring chiefdoms. Francis has been working as a CHO for 26 years and is very experienced in his field. He also has 12 community health workers (CHW) working under him. The CHWs help reach the locations that are basically isolated from the clinic.
Francis, a community health officer (CHO) and the community supervisor for the four peripheral health units (PHUs) in the neighboring chiefdoms. Francis has been working as a CHO for 26 years and is very experienced in his field. He also has 12 community health workers (CHW) working under him. The CHWs help reach the locations that are basically isolated from the clinic.
During our interview with him we asked about the main health problems he faces. Francis mentioned malaria, ARI (acute respiratory infections), trauma wounds, STIs, and malnutrition. He went on to inform us that the necessary supplies to treat malaria and ARI are not always available and that drugs to treat these issues are scarce. We asked him specifically about sickle cell and if he had ever seen any patients with the symptoms of the disease and he had not. While we are taking his answer into account we have learned that a lot of people do not know exactly what sickle cell is, and often confuse the symptoms with other diseases. Therefore, it has been hard to gauge if sickle cell patients actually are or are not in the area.
Side Note: A lesson we learned on day one was that people were getting confused when we used “sickle cell anemia” in our questions/descriptions of the project. The reason why is because when someone hears “anemia,” their mind immediately goes to nutrient-deficient anemia and not sickle cell; therefore, we have made it a point to just use “sickle cell” when talking to CHOs, CHWs, and others being interviewed.
 Back to the story, while Francis did not specifically talk about sickle cell, he did say that “misdiagnosis is a crime”. This gives us hope that if more people are aware of the prevalence of sickle cell, they would want to use the diagnostic device instead of primarily diagnosing with symptoms. He then showed us around the clinic, the delivery room, maternity room, and their lab. We also learned about a few of their clinic days, including specific days for pregnant mothers, children under 5, and EPI (The Expanded Program on Immunization; aka a vaccination day).
Back to the story, while Francis did not specifically talk about sickle cell, he did say that “misdiagnosis is a crime”. This gives us hope that if more people are aware of the prevalence of sickle cell, they would want to use the diagnostic device instead of primarily diagnosing with symptoms. He then showed us around the clinic, the delivery room, maternity room, and their lab. We also learned about a few of their clinic days, including specific days for pregnant mothers, children under 5, and EPI (The Expanded Program on Immunization; aka a vaccination day).
Back down the road, after we stopped to look at some sheep for a while, we made it to the next CHC, Kalangba. This CHC is also considered a bamok, because of its larger size, and used to be the old Makeni hospital. It was by far the largest clinic we have seen so far. The CHO, Osman, that ran the clinic was very young, and he had only been working as a CHO for a year and a half. The clinic had multiple nurses, a midwife, a traditional birthing assistant, and 25 CHWs.
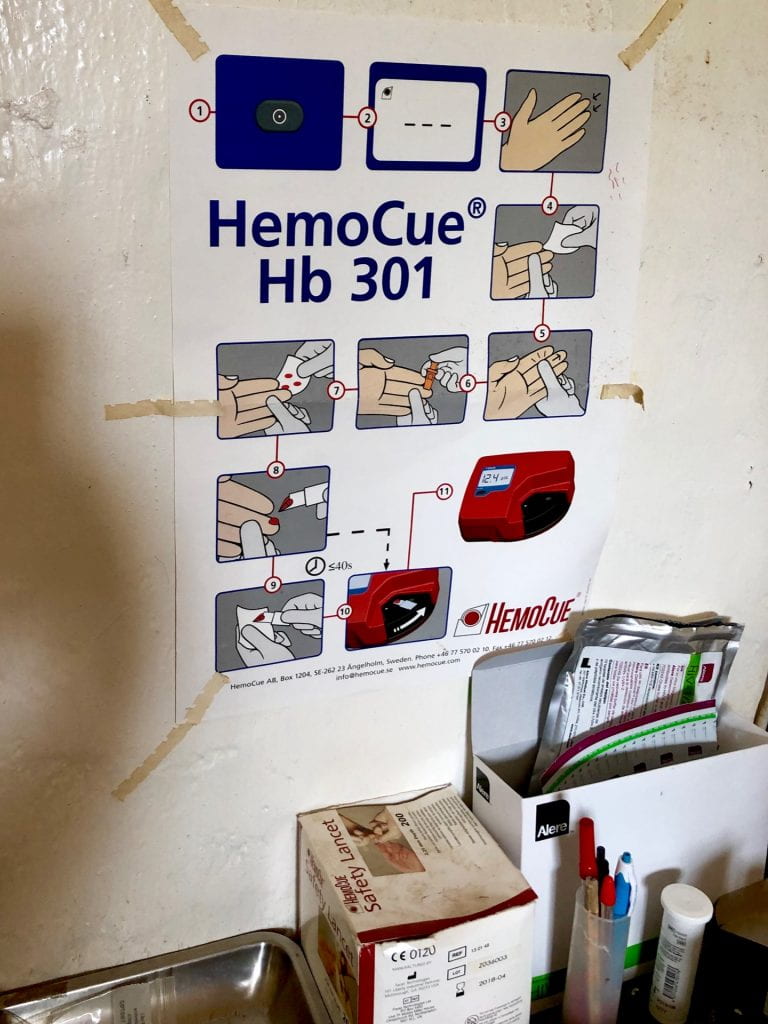
The clinic serves approximately 10 people a day and even includes home visits on Fridays. Again, like the last clinic, we did not hear a lot about sickle cell, but we did learn that they have hemoglobin levels test and a large, well-equipped (compared to the others) lab. When we visited the lab, the technician was in the middle of a malaria conformation test but was very willing to explain the other tests that are conducted in the lab, like tuberculosis conformation.
We also got to walk around their under-5 ward, ebola isolation unit (from a distance), and EPI center. Another interesting thing we saw, that was specific to the clinic, was how they recorded medical history; each patient that visited the clinic had a separate booklet and then they were organized in stacks on a shelf by their last name. Even though we were not able to learn a lot about sickle cell, it was still a great opportunity to learn about the health care system.
Once back at World Hope, we were delightfully surprised to have a meeting with Bernadette, the project manager for the anti-trafficking project for World Hope in Freetown, and the old head of the World Hope branch in Makeni. Bernadette was an incredible women to talk to. After being told at a lot of the clinics we visited that sickle cell wasn’t an issue, she reassured us that sickle cell is a large problem, especially because a lot of people do not know about its existence. She said that our device would be incredibly helpful for pregnant women and young couples for family planing (preventative measures). She gave us a really great tip to start calling sickle cell “sickler” (pronounced: sickla) at the clinics because it is the “common name” for sickle cell. While she understood that our device is in the early stages of development, she explained to us some future steps which will be needed in order to start a clinical trail next summer. Hopefully, we will be able to start using her advice, and eventually receive more of it in the future, after we advance our work in the lab.