INTRODUCTION.
Approximately 10% of males and 25% of females will experience a major depressive episode sometime during their lifetime. It is the 3rd most disabling disease in the world accounting for 70% of the psychiatric hospitalizations and 40% of the suicides. In addition to feeling sad, depressed individuals can experience a wide range of other symptoms. Chronic anxiety, emptiness, hopelessness, and worthlessness are common, as are eating and sleeping disorders. Activities that were previously pleasurable (including sex) often seem unrewarding. Low energy levels, slowness of movement, and chronic fatigue are also common as are physical symptoms that don’t respond well to treatment (such as chronic pain or digestive issues). And in some cases, cognitive and memory impairments bear a remarkable resemblance to the early stages of Alzheimer’s Disease. Depression also exacerbates other illnesses and reduces life expectancy.
In this post, I provide a brief overview of the neuroanatomy of depression. In a second post, I review some hypotheses of the causes of the brain dysfunctions underlying depression. In a third post, I describe the monoamine-related antidepressant drugs and their evolution over time. And in yet other posts, I discuss new classes of antidepressants that provide relief for many individuals that do not respond to traditional monamine antidepressants.
Where in the brain is depression located.
In what follows, I briefly present some brain structures known to be dysfunctional in depression and the specific roles they are thought to play . I also try to give you a feel for where these structures are located in the brain. For cortical structures on the surface of the brain, I use a graphic showing the left hemisphere and for structures buried inside the brain, I use a midline section.
Given the emotional, cognitive, and motor symptoms of depression, it should not be surprising that many brain areas are involved. Since the brain areas all communicate with each other, it is not clear if malfunctioning in one area is primary, or secondary to malfunctioning in another. In fact most depression symptoms likely arise from the interaction of multiple brain areas.
Cortex. Depression can be viewed as an altered state of consciousness, so it should not be surprising that the conscious part of our brain, the cerebral cortex is involved. The cortex is the convoluted grey matter providing the forebrain’s outer covering (see Figure 1, click on figures to enlarge them if text is too small).

Different parts of the cortex contribute to consciousness in different ways. Sensory cortex (green color) decodes the different types of sensory input and makes the information available to consciousness, while motor cortex (red color) directs motor output for conscious behavior. However, most of the cortex does not have well defined sensory or motor functions and is called association cortex (tan color).
One important function of association cortex is to encode long-term memories so they can be made available to consciousness. (Memories stored outside the cortex are not available to our conscious minds). Long-term cortical memory storage occurs through the creation of new synapses or the modification of existing ones. Conscious memory is also organized according to principles that facilitate recall. For example memories are stored near the sensory cortex that predominates in that memory; visual memories are stored near primary visual cortex , auditory memories near primary auditory cortex and so forth. As they are encoded, memories are also “time-stamped,” and “location-stamped” so you can typically identify when and where the memory occurred. And finally memories are also “cross-indexed” with other relevant memories providing multiple paths for retrieval. These processes are all impaired to some extent in depressed individuals.
The other important function of association cortex is to provide executive control over the planning and decision-making processes of the cortex. This role is carried out primarily by the prefrontal cortex which can attend to relevant relevant sensory input, compare that input to stored memories to decide what to do, and then direct motor cortex to perform whatever actions best achieve the desired goal. Basically the prefrontal cortex makes decisions about what you should be doing and when you should be doing it. These processes are also clearly impaired in depressed individuals. If we were to designate a part of the human brain as the “seat of consciousness” it would be the prefrontal cortex.

When a person is depressed, the prefrontal cortex exhibits a dysfunctional metabolic state called “hypofrontality” (also present in schizophrenia and other psychiatric disorders). Hypofrontality is accompanied by decreases in blood flow, neural activity, and neuronal metabolism. In some cases, there is even evidence of degeneration. As the final common pathway for conscious thought and behavior, the malfunctioning prefrontal cortex is clearly central to many depression symptoms.
As might be expected, after depression recovery, prefrontal functioning typically returns to a more normal state. Further implicating the prefrontal cortex , a depression treatment (repetitive transcranial magnetic stimulation), targets the prefrontal cortex. An even more effective, but less targeted treatment, electroconvulsive shock, is also thought to work by “jump starting” the prefrontal cortex. And finally consciousness-altering drugs, such as ketamine and other psychedelic hallucinogens, might also exert their therapeutic effects by re-activating prefrontal cortex activity. More about these treatments in a later post.

At the same time, proper functioning of the prefrontal cortex also depends upon appropriate input from other cortical structures. Two structures that have received considerable attention are the anterior cingulate cortex and the insula. The anterior cingulate cortex is buried deep in the longitudinal fissure (the deep groove in the top of the brain that separates the two hemispheres) right behind the prefrontal cortex. Among other things, the anterior cingulate cortex encodes the expectation of reward in different situations based upon experience. Its malfunctioning is thought to contribute to the depressed patient’s lack of interest in activities that were previously enjoyable. The insula, hidden inside the lateral fissure (the deep groove running horizontally on the side of the cortex) is involved in the immediate self-awareness of one’s feelings and behavior and helps filter out disruptive negative stimulation. Insula malfunctioning is thought to contribute to the increased salience of negative stimuli and the increased rumination of negative thoughts.

The limbic system and basal ganglia, two subcortical forebrain systems, are massively interconnected with the cortex, and play important roles in supporting cortical functioning. The hippocampus is essential in helping the cortex transform short-term memory (transient electrical events) into long-term memory (structural changes in cortical synapses). Without proper hippocampal functioning a person is unable to encoded new long-term memories. The hippocampal dysfunction during depression is thought to account for the Alzheimer’s-like memory deficits often seen in severely depressed individuals. In fact, one school of thought is that hippocampal degeneration may be the underlying cause of depression.

The other important limbic system structure, the amygdala, supplies emotional information to the cortex. Through experience, the amygdala assigns positive or negative value to environmental stimuli as well as to the behaviors that allow you to interact with these stimuli. This information is subsequently incorporated into long-term memories stored in the cortex. The amygdala dysfunction seen in depression is thought to contribute to the inability to experience reward as well as the enhanced negative emotional expression prevalent in depression.
The basal ganglia are a series of interconnected subcortical structures deep inside the forebrain that help the cortex plan and execute motor movements. The motor problems of both Parkinson’s and Huntington’s Diseases are caused by the selective deaths of basal ganglia neurons. While the issues appear less serious in depression, basal ganglia dysfunction is thought to contribute to the low energy levels and slowness of movement seen in Depression.
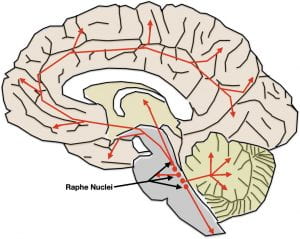
And finally, two brainstem structures that contribute are the Raphe Nuclei and Locus Coeruleus. Both are relatively small structures located in the dorsal pons of the hindbrain that house the cell bodies of neurons that release monoamine neurotransmitters. The Raphe nuclei contain the cell bodies of the brain’s serotonin-releasing neurons while the locus coeruleus contains the cell bodies of the brain’s norepinephrine-releasing neurons. In both cases, their long axons travel to virtually all areas of the brain and spinal cord where they modulate the activity of the neurons they innervate. All of the brain areas involved in depression receive input.

While neurotransmitter release by both of these systems exhibit circadian rhythms, release also increases under specific circumstances. Serotonin release increases immediately before executing body movements and are thought to prepare the different levels of the nervous system to efficiently carry out movements. Norepinephrine, on the other hand, is the neurotransmitter of “sympathetic arousal” and helps to prepare the nervous system to deal with emotion-provoking situations which also often require movement (in extreme situations: “fight or flight”).
The serotonin and norepinephrine systems target many of the same brain areas and have similar patterns of circadian release. Both also decrease their activity during depression. Consistent with the role of these systems in depression, traditional monoamine-related antidepressants are therapeutic by boosting serotonin and/or norepinephrine concentrations in the brain. However, monamine-related antidepressants don’t provide therapeutic relief for all depressed individuals, and the exact role of serotonin, norepinephrine, and perhaps dopamine, in depression is incompletely understood.
We’re not exactly sure how all these brain dysfunctions come to be. Is there an initial issue that causes all the other problems or do all the problems arise independently? In the next post, I will present some of the ideas scientists have had over the years.